Intracytoplasmic Sperm Microinjection (ICSI)
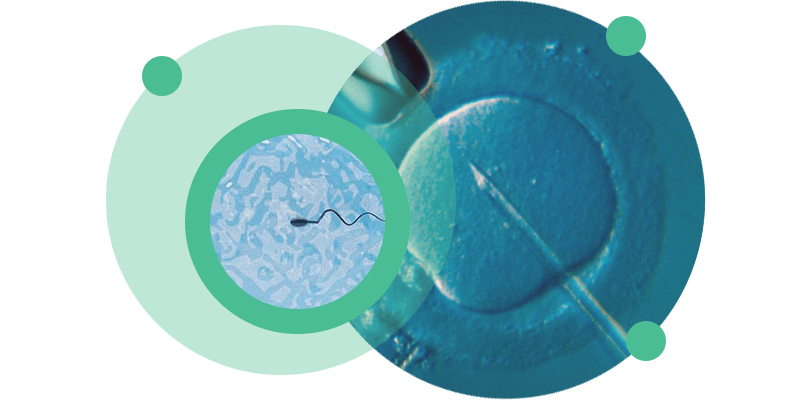
Intracytoplasmic sperm injection (ICSI) is a medically assisted procreation technique in which a pre-selected sperm is injected directly into the cytoplasm of the oocyte.
ICSI is indicated in cases of severe male infertility, fertilisation failure during previous cycles of conventional IVF or cycles intended for pre-implantation genetic diagnosis.
About ICSI
Intracytoplasmic Sperm Injection (ICSI) is a Medically Assisted Reproduction technique that has made it possible to overcome causes of infertility that conventional In Vitro Fertilisation (IVF) cannot.
Unlike conventional IVF, in which several spermatozoa are brought into contact with the oocytes, in ICSI a single spermatozoon, selected beforehand, is injected directly into the cytoplasm of the oocyte. The stages of ICSI are similar in many respects to those of conventional IVF, but ICSI requires more preparation of the oocytes and the fertilisation process requires specialised equipment, namely an inverted microscope with microinjectors, operated by joysticks, to which small pipettes are connected.
ICSI can be carried out using gametes from both members of the couple (intraconjugal ICSI) if the couple is heterosexual. Or you can use donated gametes, both oocytes and sperm.
ICSI is indicated in cases of moderate to severe male infertility:
- Low sperm concentration in the ejaculate – Oligozoospermia
- Sperm motility defects – Asthenozoospermia
- High percentage of morphological defects – Teratozoospermia
- Absence of spermatozoa in the ejaculate – Azoospermia – in these cases, a testicular biopsy and ICSI with sperm recovered from testicular tissue are indicated.
ICSI is also indicated in situations where fertilisation has failed during previous cycles of conventional IVF and/or intrauterine insemination, and in cases where pre-implantation genetic diagnosis (PGD) will be carried out on the embryos obtained.
Although each case is treated individually and on a personalised basis by our clinical team, we present here the general stages of an ICSI treatment.
Ovarian stimulation
After medical consultation and definition of the best protocol to follow, the woman’s ovaries begin to be stimulated from the 2nd day of her period. Stimulation is carried out using injectable hormonal drugs that stimulate the growth of several follicles simultaneously, unlike the natural cycle in which, as a general rule, only one reaches the level of development required for fertilisation. The medication used can be administered by you at home.
After the start of treatment, the growth of the follicles is monitored by ultrasound scans at intervals of around 3 days. When a reasonable number of follicles are at the pre-ovulatory stage (larger than 17 mm on ultrasound), another hormonal drug (hCG) is administered, which will cause the final maturation of the follicles and the oocytes they contain, as would occur in a natural cycle.
Follicular puncture
36 hours after taking the hCG hormone, a follicular puncture is performed. This is a rapid surgical procedure, performed vaginally and under sedation, during which liquid is drawn from the follicles using a needle monitored by ultrasound.
From this point onwards, depending on the protocol defined, you may start taking new medications (oral or vaginal) to help the uterus become more receptive to receiving embryos and to allow them to implant.
Gamete processing
The follicular fluid arrives at the laboratory and the presence of oocytes is observed. These oocytes are collected and processed to make ICSI possible, i.e. all the cells surrounding the oocyte are removed in a procedure called denudation. The stripping allows the maturity and quality of the oocytes to be assessed, and only mature oocytes will be able to be fertilised.
On the same day as the follicular puncture and at around the same time, the ejaculate sample must be collected by masturbation. The sample may be collected on the clinic’s premises or at home, provided that it is delivered to the clinic by the patient. The ejaculate sample is treated with appropriate media that favour the selection of spermatozoa with normal morphology and motility. The processing of cryopreserved ejaculate or testicular tissue samples follows the same principles as the processing of ‘fresh’ ejaculate samples.
ICSI
Once the oocytes and spermatozoa have been processed, the microinjection procedure is prepared. This is done using an inverted microscope equipped with two microinjectors operated using joysticks (micromanipulators) into which small pipettes are placed. One of the pipettes will hold the oocyte so that the other pipette can inject the selected sperm directly into the oocyte’s cytoplasm.
Fertilisation and embryo culture
16 to 18 hours after microinjection, fertilisation is confirmed by the presence of two pronuclei (one female and one male), which fuse over the following hours and give rise to embryos through successive cell divisions. The embryos remain in culture in incubators with a suitable atmosphere and in culture media that encourage their development. The progress of the embryos is assessed on a daily basis.
Embryo transfer and/or cryopreservation
3 to 5 days after microinjection, the best quality embryo or embryos are transferred to the patient’s uterus. Embryo transfer is a rapid procedure without analgesia/sedation, in which one or more embryos are introduced into the uterine cavity using a catheter specifically designed for this purpose.
If it is not possible to transfer embryos in the cycle in which they were created (due to the risk of ovarian hyperstimulation syndrome or for any other reason) or if there are more good quality embryos than can be transferred, these embryos are cryopreserved.
bHCG analysis
12 days after the embryo transfer, a blood sample is taken to detect the pregnancy hormone bHCG.
The success rate for ICSI, both nationally and internationally, is around 30%.
The success rate is influenced by various factors, the most important of which are the woman’s age, the quality of the eggs and the quality of the sperm. You should therefore discuss your individual case with your doctor.
Common Questions
Taking into account all the stages of the treatment, including ovarian stimulation and transfer of the embryos into the uterus, the elapsed time varies between 15 and 20 days.
Ovarian stimulation takes an average of 8 to 15 days. The duration depends on the protocol used and each woman’s specific ovarian response.
The woman’s age influences the success of the technique in terms of both the quantity and quality of the oocytes collected. We know that a woman’s reproductive potential diminishes considerably after the age of 35 and drops sharply after the age of 40. From these ages onwards, it is more likely that the oocytes will be affected by chromosomal abnormalities, which have a negative impact on the fertilisation rate and embryonic development.
It’s recommended that you rest for two days, abstain from sexual relations for 5 days and avoid strenuous physical activity until the pregnancy test has been carried out (12 days after the transfer).
The treatment does not cause any pain, just some discomfort on the day the ovaries are punctured to collect the oocytes. The follicular puncture procedure itself does not cause any discomfort as it is carried out under sedation.
The greatest risk, although rare, is that of ovarian hyperstimulation, which will subsequently require appropriate care but which, with vigilance, will usually resolve spontaneously. Close ultrasound monitoring after the start of ovarian stimulation can considerably reduce the occurrence of these situations.
Once treatment has begun, the patient will need to visit the clinic every 2 or 3 days for an ovarian stimulation ultrasound check and, on average, 2 to 4 ultrasounds are performed until follicular puncture is scheduled.
On the day of the follicular puncture, the husband/partner will also have to come to the clinic to collect the ejaculate, unless he already has sperm or cryopreserved testicular tissue.
The ejaculate sample can be taken at home, provided that it can be delivered to the clinic’s premises by you 30 to 45 minutes after the sample has been taken. During transport, the container containing the sample should be kept close to the body to avoid large fluctuations in temperature. The collection container can be supplied by the CETI or a urine collection container can be purchased from any pharmacy.
You can consult the CETI price list here.
